
Osteoarthritis is a degenerative joint pathology, accompanied by dystrophy processes of the cartilaginous tissues. As the disease progresses, the joint bag, the ligamentous apparatus, the synovium, and the closest bone structures also participate in the destructive process.
Prevalence of osteoarthritis
Most people with osteoarthritis are elderly. Disease after the age mark of 65 is not only the most frequently diagnosed joint pathology, but also the main reason for disability with subsequent disability. Also, in old age, most women are ill, but among young people, most of the ill are men.
In different countries, the incidence of osteoarthritis varies greatly. It has not yet been possible to establish the reasons for the wide dissemination of statistical data.
Causes and risk factors
Osteoarthritis is a disease that can be primary or secondary. If there are no objective reasons for the development of pathology, they speak of the primary type. If it was possible to identify the causes of arthrosis, they speak of the secondary type.
Secondary osteoarthritis can be triggered by the following negative factors:
- joint traumatization of various kinds (frequent falls, sprains, bruises);
- chronic congenital tissue dysplasia;
- pathological changes in metabolic processes;
- various autoimmune pathologies;
- nonspecific inflammatory processes in the joint area;
- some pathologies of the organs of the endocrine system;
- degenerative-dystrophic processes that occur chronically;
- various diseases, accompanied by excessive joint mobility, together with a weak ligamentous apparatus;
- presence of hemophilia;
- specific type of inflammatory processes.
In addition to the immediate causes, the action of which leads to the development of osteoarthritis, there are also predisposing factors that do not cause the disease by themselves, but can increase the risk of its development.

These include:
- is over 55 years old;
- excess weight, due to which increases the load on the articular joints;
- excessive load on a joint or group in case of inappropriate sports training, specific work that requires a prolonged stay in one position;
- history of joint surgery;
- inheritance;
- hormonal changes in the female body in postmenopause;
- constant hypothermia;
- pathologies of the spine that are not treated;
- Insufficient intake of useful microelements and macroelements with food.
Development Mechanism
The mechanism of development of osteoarthritis is well known. Cartilage, which ensures the normal contact of two bones, is naturally smooth, without irregularities or roughness, which helps to maintain the normal movement of the joints. With a disease, the structure of the cartilage changes, it becomes rough, defects appear that reduce the effectiveness of natural sliding.
Due to the acquired irregularity, the cartilage is gradually injured, in places it begins to calcify and in places it ossifies. In this case, it is possible to separate small particles that end up in the joint fluid and can damage the surrounding tissues.
As the pathology worsens, the joint may enter a state of chronic subluxation, significantly impairing its motor function.
Degrees
Doctors divide osteoarthritis into three main grades:
- I grade.It is characterized by the absence of a clear clinical picture. The patient may have rare complaints of pain in the affected joint, but usually does not consult a doctor. At the same time, changes in the ligamentous muscle apparatus and joint fluid are observed, but there are still no visible deformities.
- II degree.The symptoms of osteoarthritis become more pronounced. The pain is characterized by being bearable, but it occurs regularly. The patient goes to the doctor, since he notices a decrease in the quality of life. A characteristic crunch can be heard in the affected joint. Changes are observed in nearby muscle structures, as nerve conduction is impaired.
- III degree.Characterized by pronounced signs. Articular cartilage is very thin, cysts, calcification or ossification foci can be found in it. The ligamentous apparatus is shortened, which leads to increased mobility in the affected area, which is accompanied by a restriction due to a pronounced inflammatory process. The metabolism of the surrounding tissues is affected, which can lead to muscular dystrophy.
In any case, the patient must clarify the diagnosis of the treating physician. This is due to the specificity of the course of the disease, which is characterized by stages of remission and exacerbation, which alternately replace each other.
Pain with disease

Pain in osteoarthritis is the most common complaint with which patients go to the doctor. Its characteristic feature is its connection with the time of day, the weather, physical activity.
In most patients, pain is aggravated by walking, running, or other types of physical activity directed at the affected joint. As soon as the load stops, the pains gradually subside. Its development is explained by the fact that cartilage can no longer perform its shock absorption functions.
At night, discomfort occurs most often as a result of stagnation of blood in the veins. Another reason is the increase in intraosseous pressure during this period.
One of the main diagnostic criteria is the presence of the so-called initial pains that bother the patient at the moment when active movement has just begun. The initial pains usually go away if you continue physical activity. Its appearance is explained by the presence of joint deposits (debris) that irritate the nerve endings. As soon as these deposits move away from the nerves, the pain disappears.
Symptoms
In addition to pain, doctors identify other signs of osteoarthritis for which pathology can be suspected.
These include:
- Pains and cracking sound.Lomota appears mainly in the event that a person has received hypothermia. At first, the crackling will be barely audible, but as the disease progresses without therapy, it will be audible to the people around you.
- Decreased ability to move. At an early stage of the development of pathology, there is no decrease in mobility. However, the longer the disease remains untreated, the stronger the limitation of movement in the joint becomes. This is explained by the narrowing of the joint space and the spasm of the closest muscle structures.
- Joint deformity.It is characteristic of the late stage of osteoarthritis, but it is also an important indicator of the course of the disease. During this period, it is already very difficult to treat the disease.
What doctor treats osteoarthritis?
Who treats osteoarthritis? In most cases, several specialists are involved in therapy. First, an arthrologist, a specialist in joints, intervenes. In addition, the patient will also need to visit an orthopedist. If the disease is a consequence of an inflammatory process, it is also recommended to visit a rheumatologist.
If necessary, other specialists can participate during treatment. Most often, you need to resort to the services of traumatologists, physical therapists, masseurs, surgeons.
Diagnosis
Treatment of osteoarthritis of the joints begins only after the diagnosis is confirmed and the degree of pathology established. First of all, the doctor interviews the patient in detail and conducts an examination. The presence of characteristic complaints and deformities suggests that a disease exists.
Radiography of the affected joint is a mandatory way to confirm the diagnosis. If the disease affects the knee, a picture of the knee is taken, if the pathology is in the hand, radiological signs of the disease are specifically looked for there.
X-ray diagnosis does not always give sufficient results to diagnose the patient. In this case, it can be sent to an MRI (this will allow to assess the state of the soft tissues and their participation in the pathological process) or a computed tomography (this will allow to draw conclusions about the state of the bone and cartilaginous structures, the participationof the closest anatomical structures in the pathological process).
Treatment
How to treat osteoarthritis of the joints? The choice of the appropriate therapeutic technique depends on the severity of the symptoms and the stage of the disease.
The physician selects the therapy regimen after assessing the general condition of the patient and the course of the disease. Both conservative and surgical treatment methods can be used.
Medications
How to treat a disease if it is preferable not to surgery, but to use drugs?
Conservative therapy is suitable for patients only at an early stage of pathology formation and will include the use of three main groups of drugs:
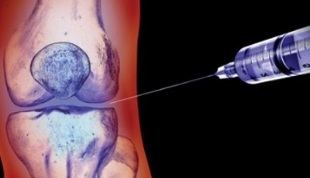
- glucocorticosteroids- hormonal drugs that effectively relieve the inflammatory process during an exacerbation are injected into the joint cavity;
- nonsteroidal anti-inflammatory drugs,which are injected and injected mainly into the muscles near the joint or directly into a vein. But doctors can also recommend pills, although this option for taking NSAIDs is undesirable due to the negative effect on the gastrointestinal tract;
- chondroprotectors- drugs of this group can reduce the destruction of cartilage tissue and improve regeneration, they are especially effective in the initial stages of the formation of the disease.
Surgical
How to cure osteoarthritis, if the disease has gone far enough? In this case, conservative therapy will be ineffective, and doctors can only recommend surgery to the patient.
Today, joint replacement is done in most cases. During the operation, the actual joint is replaced with a prosthesis, which has all the functions of a healthy joint.
In some cases, palliative therapy options are provided, the main task of which is to reduce the load on the articular surfaces.
Exercise
In the early stages of the disease, it is treated not only with drugs, but also with physical therapy exercises. Exercise is an important stage of therapy that helps maintain joint functionality and reduces the likelihood of further disease progression.
Depending on the severity of the pathology and the individual characteristics of the patient, the set of exercises is selected individually. The doctor must take into account the location of the osteoarthritis, which allows the most effective effect on the affected tissues.
Self-study without medical supervision is not recommended, especially in the initial stage. Exercises should be selected to be as gentle as possible, without sudden movements.
Exercise therapy classes are effective only if the patient spends a little time on the recommended complex every day.
Traditional methods

Many people with osteoarthritis refuse to use medicine or surgery until the last minute. In this case, alternative drugs are used as substitutes for drugs.
The plants most used in therapy are:
- Kalanchoe;
- ginger;
- hell;
- bay leaf;
- garlic;
- cinnamon;
- ponytail and others.
They are used in the form of tinctures, decoctions, poultices on the affected area. It is important to note that a complete treatment of the disease using only homemade recipes is impossible. It is better if traditional therapies are combined with traditional medicine.
Prevention
What to do to reduce the probability of developing osteoarthritis in old age? Simple preventive measures are available to anyone.
Recommended:
- Moderate daily physical activity: walking, cycling, doing simple exercises such as loading, etc.
- adherence to the basic principles of a healthy diet: eat frequently, but little by little, avoid fast food, overeat, heavy and fatty foods, eat a lot of spices;
- weight control: weight gain causes increased stress on the joints, which can lead to osteoarthritis;
- timely treatment of chronic diseases leading to metabolic disorders;
- the use of vitamin and mineral complexes in case the amount of nutrients provided with food is considered insufficient.
Difference between arthritis and osteoarthritis
Many people confuse arthritis and osteoarthritis due to the similarity of the sound. However, these are completely different diseases.
Arthritis is not called dystrophy and degeneration in the joint tissues, but any inflammatory reaction that can develop in the joint cavity, regardless of its cause. Inflammation most often affects not only the joint, but also the closest muscles, bones, and ligamentous structures. Pain in arthritis is not associated with physical activity, it can bother the patient even at rest, and there is no creaking in the joints.

In most cases, it is impossible to independently distinguish arthritis from osteoarthritis, since the main symptom is pain and patients rarely have an idea of its characteristics for each of the pathologies.
It is better to entrust the establishment of an accurate diagnosis to the attending physician so as not to make mistakes with the subsequent treatment and prevention of the disease.
Osteoarthritis is a serious disease that can lead to disability if the patient does not see a doctor in time. At the first signs of the disease, it is recommended to contact a specialist to confirm the diagnosis and select the most optimal treatment.
If it is possible to contract the disease at an early stage of development, then surely it will be possible to do so even without surgical intervention, limiting itself only to conservative treatment.



































